Page 575 - TNFlipTest
P. 575
Toronto Notes 2019 Venous Thromboembolism Venous Thromboembolism
Definition
• thrombusformationandsubsequentinflammatoryresponseinasuperficialordeepvein
• superficial thrombophlebitis, deep vein thrombosis (DVT), and pulmonary embolism (PE)
• thrombi propagate in the direction of blood flow (commonly originating in calf veins)
• more common in lower extremity than upper extremity
• incidence ~1% if age >60 yr
• most important sequelae are pulmonary embolism (~50% chance with proximal DVT) and chronic
venous insufficiency
Etiology (Virchow’s Triad)
• endothelialdamage
■ exposes endothelium to prompt hemostasis
■ leads to decreased inhibition of coagulation and local fibrinolysis
• venousstasis
■ immobilization (post-MI, CHF, stroke, and post-operative) inhibits clearance and dilution of
coagulation factors • hypercoagulability
■ inherited (see Hypercoagulable Disorders, H33) ■ acquired
◆ age (risk increases with age)
◆ surgery (especially orthopedic, thoracic, GI, and GU)
◆ trauma (especially fractures of spine, pelvis, femur or tibia, and spinal cord injury)
◆ neoplasms (especially lung, pancreas, colon, rectum, kidney, and prostate)
◆ blood dyscrasias (myeloproliferative neoplasms, especially PV, ET), PNH, and hyperviscosity
(multiple myeloma, polycythemia, leukemia, and sickle cell disease)
◆ prolonged immobilization (CHF, stroke, MI, and leg injury)
◆ hormone related (OCP, HRT, and SERMs)
◆ pregnancy
◆ APS
◆ heart failure (risk of DVT greatest with right heart failure and peripheral edema)
• idiopathic(10-20%arelaterfoundtohavecancer)
Clinical Features of DVT
• absenceofphysicalfindingsdoesnotruleoutdisease
• unilaterallegedema,erythema,warmth,andtenderness;purple-bluecolour
• palpablecord(thrombosedvein)
• phlegmasia alba dolens (white appearance) and phlegmasia cerula dolens (acute pain and edema) with
massive thrombosis
• Homan’ssign(painwithfootdorsiflexion)isunreliable
Differential Diagnosis of DVT
• musclestrainortear,lymphangitisorlymphobstruction,venousvalvularinsufficiency,ruptured popliteal cysts, cellulitis, and arterial occlusive disease
Investigations for DVT
• D-dimertestonlyusefultoruleoutDVTifnegativewithlowclinicalsuspicionofdiseaseandnoother acute medical issues
• dopplerultrasoundismostusefuldiagnostictestforDVT ■ sensitivity and specificity for proximal DVT ~95%
■ sensitivity for calf DVT ~70%
• othernon-invasivetestsincludeMRIandimpedenceplethysmography
• venographyisthegoldstandard,butisexpensive,invasive,andhigherrisk
• CTPA or V/Q scan if PE suspected
Post-Thrombotic Syndrome
• developmentofchronicvenousstasissignsandsymptomssecondarytoadeepvenousthrombosis • symptoms:pain,venousdilatation,edema,pigmentation,skinchanges,andvenousulcers
• clinical severity can be estimated based on the Villalta score
• large impact on quality of life following a DVT
• treatment:extremityelevation,exercise,continuouscompressionstockings,intermittentpneumatic compression therapy, and skin/ulcer care
• forclinicalfeaturesandtreatmentofPE,seeRespirology,R18
Hematology H35
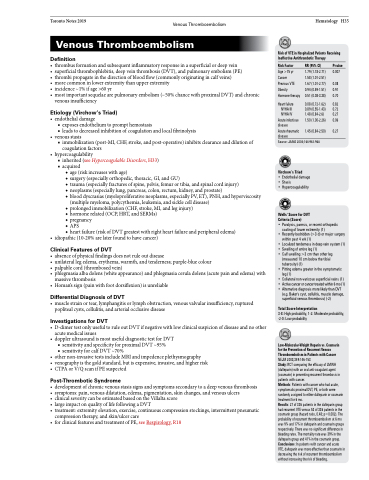
Risk of VTE in Hospitalized Patients Receiving Ineffective Antithrombotic Therapy
Risk Factor
Age >75 yr Cancer
Previous VTE Obesity Hormone therapy
Heart failure NYHA III NYHA IV
Acute infectious disease
Acute rheumatic disease
RR (95% CI) P-value
1.79 (1.18-2.71) 0.007 1.58 (1.01-2.51)
1.67 (1.01-2.77) 0.08 0.94 (0.59-1.51) 0.91 0.51 (0.08-3.38) 0.70
0.08 (0.72-1.62) 0.82 0.89 (0.55-1.43) 0.72 1.48 (0.84-2.6) 0.27 1.50 (1.00-2.26) 0.06
1.45 (0.84-2.50) 0.27
Source: JAMA 2004;164:963-968
Virchow’s Triad
• Endothelial damage • Stasis
• Hypercoagulability
Wells' Score for DVT Criteria (Score)
• Paralysis, paresis, or recent orthopedic
casting of lower extremity (1)
• Recently bedridden (>3 d) or major surgery
within past 4 wk (1)
• Localizedtendernessindeepveinsystem(1)
• Swelling of entire leg (1)
• Calf swelling >3 cm than other leg
(measured 10 cm below the tibial
tuberosity) (1)
• Pitting edema greater in the symptomatic
leg (1)
• Collateral non-varicose superficial veins (1)
• Activecancerorcancertreatedwithin6mo(1)
• AlternativediagnosismorelikelythanDVT
(e.g. Baker's cyst, cellulitis, muscle damage, superficial venous thrombosis) (-2)
Total Score Interpretation
3-8: High probability, 1-2: Moderate probability, -2-0: Low probability
Low-Molecular-Weight Heparin vs. Coumarin for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer NEJM 2003;349:146-153
Study: RCT comparing the efficacy of LMWH (dalteparin) with an oral anti-coagulant agent (coumarin) in preventing recurrent thrombosis in patients with cancer.
Methods: Patients with cancer who had acute, symptomatic proximal DVT, PE, or both were randomly assigned to either dalteparin or coumarin treatment for 6 mo.
Results: 27 of 336 patients in the dalteparin group had recurrent VTE versus 53 of 336 patients in the coumarin group (hazard ratio, 0.48; p=0.002). The probability of recurrent thromboembolism at 6 mo was 9% and 17% in dalteparin and coumarin groups respectively. There was no significant difference in bleeding rates. The mortality rate was 39% in the dalteparin group and 41% in the coumarin group. Conclusions: In patients with cancer and acute VTE, dalteparin was more effective than coumarin in decreasing the risk of recurrent thromboembolism without increasing the risk of bleeding.