Page 577 - TNFlipTest
P. 577
Toronto Notes 2019 Hematologic Malignancies and Related Disorders
◆ post-operatively: IV heparin, LMWH, DOAC can be used for anticoagulation (consult with surgeon prior to re-initiation)
◆ for patients at high risk for thromboembolism (VTE <12 wk, recurrent VTE, antiphospholipid antibody syndrome, atrial fibrillation with prior stroke, and mechanical heart valve), IV heparin or LMWH (bridging) should be given before and after the procedure while the INR is below 2.0
Prophylaxis
• considerforthosewithamoderatetohighriskofthrombosiswithoutcontraindications
• non-pharmacologicalmeasuresinclude:earlyambulation,elasticcompressionstockings(TEDs),and
intermittent pneumatic compression (IPC)
• UFH5,000IUSCbid,UFH5,000IUSCtidorLMWHasperhospitalprotocol(e.g.enoxaparin40mg
SC daily, dalteparin 5000 U SC qid), and DOACs for orthopedic surgery thromboprophylaxis
Contraindications and Adverse Reactions of Anticoagulant Therapy
• absolute:activebleeding,severebleedingdiathesis,orplatelets<20-30x109/L(<20,000/mm3), intracranial bleeding, and neuro or ocular surgery within <10 d
• relative: mild-moderate neurologic diathesis or thrombocytopenia, brain metastases, recent major trauma, major abdominal surgery within past 2 d, GI/GU bleed within 14 d, endocarditis, severe HTN (sBP >200 or dBP >120), and recent stroke
Hematology H37
Table 30. Contraindications of Anticoagulant Therapy
Absolute Contraindications to Treatment
Active bleeding
Severe bleeding diathesis or platelet count <20 x 109/L (<20,000/mm3)
Intracranial bleeding
Neurosurgery or ocular surgery within 10 d
Treatment of Pulmonary Embolism
Relative Contraindications to Treatment
Mild-moderate bleeding diathesis or thrombocytopenia Brain metastases
Recent major trauma
Recent stroke
Major abdominal surgery within past 2 d GI/GU bleeding within 1-4 d
Endocarditis
Severe hypertension (sBP >200 or dBP >120)
Typical Age of Presentation of Leukemias
• ALL: Children and older adults • CML: 40-60 yr
• AML, CLL: >60 yr
Leukemia: malignant cells arise in bone marrow and may spread elsewhere (including blood, lymph nodes, and lymphoid tissue) Lymphoma: malignant cells arise in lymph nodes and lymphoid tissues and may spread elsewhere (including blood and bone marrow) BUT the location where the malignant cells are found does not solely define the type of hematologic malignancy – classified based on the characteristics of the cell (histology, histochemistry, immunophenotyping, cytogenetics, molecular changes)
• seeRespirology,R18
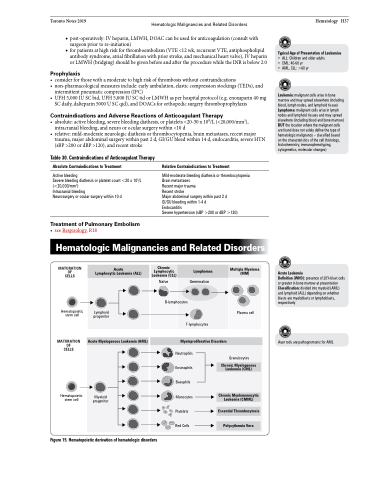
Hematologic Malignancies and Related Disorders
MATURATION OF CELLS
Hematopoietic stem cell
MATURATION OF CELLS
Hematopoietic stem cell
Acute Leukemia
Definition (WHO): presence of 20% blast cells or greater in bone marrow at presentation Classification: divided into myeloid (AML) and lymphoid (ALL) depending on whether blasts are myeloblasts or lymphoblasts, respectively
Auer rods are pathognomonic for AML
Acute Lymphocytic Leukemia (ALL)
Chronic Lymphocytic Leukemia (CLL)
Lymphomas
Multiple Myeloma (MM)
Germination ocytes
T-lymphocytes
Lymphoid progenitor
Naïve B-lymph
Plasma cell
Acute Myelogenous Leukemia (AML)
Myeloproliferative Disorders
Neutrophils Eosinophils Basophils Monocytes Platelets Red Cells
Granulocytes
Polycythemia Vera
Chronic Myelogenous Leukemia (CML)
Chronic Myelomonocytic Leukemia (CMML)
Myeloid progenitor
Essential Thrombocytosis
Figure 15. Hematopoietic derivation of hematologic disorders