Page 58 - TNFlipTest
P. 58
A24 Anesthesia
Pain Management Toronto Notes 2019
Confusion and Agitation
• ABCsfirst–confusionoragitationcanbecausedbyairwayobstruction,hypercapnea,hypoxemia • neurologicstatus(GlasgowComaScale,pupils),residualparalysisfromanesthetic
• pain,distendedbowel/bladder
• fear/anxiety/separationfromcaregivers,languagebarriers
• metabolicdisturbance(hypoglycemia,hypercalcemia,hyponatremia–especiallypost-TURP) • intracranialcause(stroke,raisedintracranialpressure)
• drug effect (ketamine, anticholinergics, serotonin)
• elderly patients are more susceptible to post-operative delirium
Respiratory Complications
• susceptibletoaspirationofgastriccontentsduetoPONVandunreliableairwayreflexes
• airwayobstruction(secondarytoreducedmuscletonefromresidualanesthetic,softtissuetraumaand
edema, or pooled secretions) may lead to inadequate ventilation, hypoxemia, and hypercapnia
• airwayobstructioncanoftenberelievedwithheadtilt,jawelevation,andanteriordisplacementofthe
mandible. If the obstruction is not reversible, a nasal or oral airway may be used
Hypotension
• mustbeidentifiedandtreatedquicklytopreventinadequateperfusionandischemicdamage
• reducedcardiacoutput(hypovolemia,mostcommoncause)and/orperipheralvasodilation(residual
anesthetic agent)
• firststepintreatmentisusuallytheadministrationoffluids±inotropicagents
Hypertension
• pain, hypercapnia, hypoxemia, increased intravascular fluid volume, and sympathomimetic drugs can cause hypertension
• IVnitroglycerin,hydralazine,calciumchannelblockersorβ-blockingdrugs(e.g.esmololand metoprolol) can be used to treat hypertension
Pain Management
Definitions
• pain: perception of nociception, which occurs in the brain
• nociception: detection, transduction, and transmission of noxious stimuli
Pain Classifications
• temporal:acutevs.chronic
• mechanism:nociceptivevs.neuropathic
Acute Pain
• painofshortduration(<6wk)usuallyassociatedwithsurgery,trauma,oracuteillness;oftenassociated with inflammation
• usuallylimitedtotheareaofdamage/traumaandresolveswithhealing
Risk Factors for Post-Operative Nausea and Vomiting (PONV)
• Young age
• Female
• History of PONV
• Non-smoker
• Type of surgery: ophtho, ENT, abdo/pelvic,
plastics
• Type of anesthetic: N2O, opioids, volatile
agents
Drugs for Preventing Post-Operative Nausea and Vomiting
Cochrane DB Syst Rev 2006;3:CD004125 Purpose: To evaluate the efficacy of antiemetics in preventing PONV.
Methods: A meta-analysis was performed looking at randomized controlled trials comparing an antiemetic to either a second antiemetic or placebo. Trials looking at dosing and/or timing of medication administration were also included. PONV was used as the primary outcome.
Results: 737 studies involving 103,237 patients. Eight drugs significantly reduced the occurence
of PONV, namely: droperidol, metoclopramide, ondansetron, tropisetron, dolasetron, dexamethasone, cyclizine, and granisetron. Relative risk (RR) versus placebo varied
between 0.60, and 0.80. Side effects included
a significant increase in drowsiness for droperidol (RR 1.32) and headache for ondansetron (RR 1.16). The cumulative number needed to treat was 3.57. Conclusion: Antiemetic medication is effective
for reducing the occurrence of PONV. However, further investigation needs to be done to determine whether antiemetics can cause more severe (and likely rare) side effects, which could alter how liberally they are used.
© Paul Kelly 2011
© Andrew Q. Tran 2014
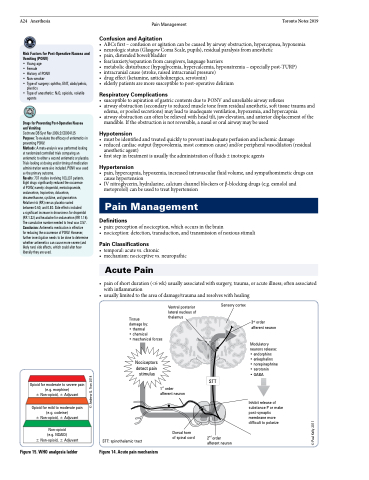
Opioid for moderate to severe pain (e.g. morphine)
± Non-opioid, ± Adjuvant
Opioid for mild to moderate pain (e.g. codeine)
± Non-opioid, ± Adjuvant
Non-opioid
(e.g. NSAID)
± Non-opioid, ± Adjuvant
Tissue
damage by:
• thermal
• chemical
• mechanical forces
Nociceptors detect pain stimulus
STT: spinothalamic tract
STT
3rd order afferent neuron
Modulatory neurons release: • endorphins
• enkephalins
• norepinephrine • serotonin
• GABA
Inhibit release of substance P or make post-synaptic membrane more difficult to polarize
Figure 15. WHO analgesia ladder
Figure 14. Acute pain mechanism
Ventral posterior lateral nucleus of thalamus
Sensory cortex
1st order afferent neuron
Dorsal horn of spinal cord
2nd order afferent neuron