Page 56 - TNFlipTest
P. 56
A22 Anesthesia
Local Anesthesia
Toronto Notes 2019
■ cardiac lesion with fixed output states (severe mitral/aortic stenosis)
■ lack of IV access
• relativecontraindications
■ pre-existing neurological disease (demyelinating lesions)
■ previous spinal surgery, severe spinal deformity
■ prolonged surgery
■ major blood loss or maneuvers that can compromise reaction
Peripheral Nerve Blocks
• depositionofLAaroundthetargetnerveorplexus
• ultrasoundguidanceandperipheralnervestimulation(needlewillstimulatetargetnerve/plexus)may
be used to guide needle to target nerve while avoiding neural trauma or intraneural injection
• mostmajornervesornerveplexicanbetargeted(brachialplexusblock,femoralnerveblock,sciatic
nerve block, etc.)
• performedwithstandardmonitors
• approximately2-4per10,000riskoflateneurologicinjury
• resuscitationequipmentmustbeavailable
Contraindications to Peripheral Nerve Blockade
• absolutecontraindications ■ allergy to LA
■ patient refusal
• relativecontraindications
■ certain types of pre-existing neurological dysfunction (e.g. ALS, MS, diabetic neuropathy) ■ local infection at block site
■ bleeding disorder
Local Anesthesia
Local Anesthetic Agents
• seeTable14,forlistofLAagents
Definition and Mode of Action
• LAaredrugsthatblockthegenerationandpropagationofimpulsesinexcitabletissues:nerves,skeletal muscle, cardiac muscle, brain
• LA bind to receptors on the cytosolic side of the Na+ channel, inhibiting Na+ flux and thus blocking impulse conduction
• differenttypesofnervefibresundergoblockadeatdifferentrates
Absorption, Distribution, Metabolism
• LAreadilycrossestheblood-brainbarrier(BBB)onceabsorbedintothebloodstream
• ester-typeLA(procaine,tetracaine)arebrokendownbyplasmaandhepaticesterases;metabolites
excreted via kidneys
• amide-typeLA(lidocaine,bupivicaine)arebrokendownbyhepaticmixed-functionoxidases(P450
system); metabolites excreted via kidneys
Selection of LA
• choiceofLAdependson:
■ onset of action: influenced by pKa (the lower the pKa, the higher the concentration of the base form
of the LA, and the faster the onset of action)
■ duration of desired effects: influenced by protein binding (longer duration of action when protein
binding of LA is strong)
■ potency: influenced by lipid solubility (agents with high lipid solubility penetrate the nerve
membrane more easily)
■ unique needs (e.g. sensory blockade with relative preservation of motor function by bupivicaine at
low doses)
■ potential for toxicity
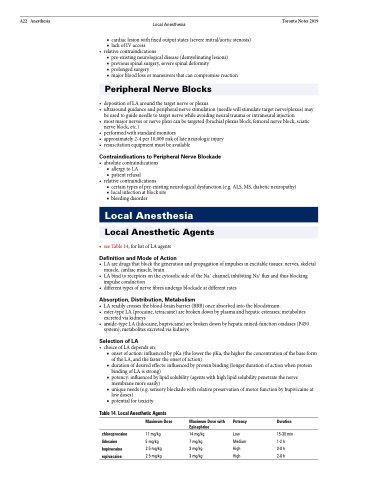
Table 14. Local Anesthetic Agents
chloroprocaine lidocaine bupivacaine ropivacaine
Maximum Dose
11 mg/kg 5 mg/kg 2.5 mg/kg 2.5 mg/kg
Maximum Dose with Potency Epinephrine
14 mg/kg Low
7 mg/kg Medium 3 mg/kg High
3 mg/kg High
Duration
15-30 min 1-2 h
3-8 h
2-8 h