Page 640 - TNFlipTest
P. 640
ID40
Infectious Diseases
Helminths
Toronto Notes 2019
1
Helminths
Roundworms – Nematodes
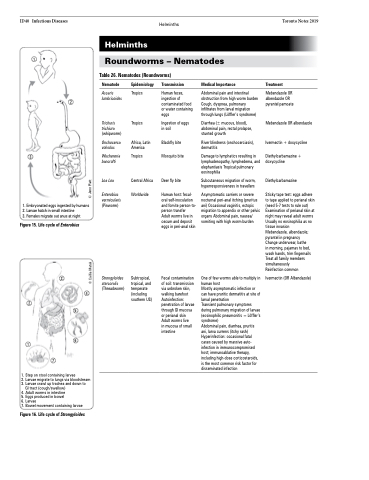
Table 26. Nematodes (Roundworms)
2
Nematode
Ascaris lumbricoides
Trichuris trichiura (whipworm)
Onchocerca volvulus
Wuchereria bancrofti
Loa Loa
Enterobius vermicularis (Pinworm)
Strongyloides stercoralis (Threadworm)
Epidemiology
Tropics
Tropics
Africa, Latin America
Tropics
Central Africa Worldwide
Transmission
Human feces, ingestion of contaminated food or water containing eggs
Ingestion of eggs in soil
Blackfly bite Mosquito bite
Deer fly bite
Human host: fecal- oral self-inoculation and fomite person-to- person transfer
Adult worms live in cecum and deposit eggs in peri-anal skin
Fecal contamination of soil: transmission via unbroken skin, walking barefoot Autoinfection: penetration of larvae through GI mucosa or perianal skin Adult worms live
in mucosa of small intestine
Medical Importance
Abdominal pain and intestinal obstruction from high worm burden Cough, dyspnea, pulmonary infiltrates from larval migration through lungs (Löffler’s syndrome)
Diarrhea (± mucous, blood), abdominal pain, rectal prolapse, stunted growth
River blindness (onchocerciasis), dermatitis
Damage to lymphatics resulting in lymphadenopathy, lymphedema, and elephantiasis Tropical pulmonary eosinophilia
Subcutaneous migration of worm, hyperresponsiveness in travellers
Asymptomatic carriers or severe nocturnal peri-anal itching (pruritus ani) Occasional vaginitis, ectopic migration to appendix or other pelvic organs Abdominal pain, nausea/ vomiting with high worm burden
One of few worms able to multiply in human host
Mostly asymptomatic infection or can have pruritic dermatitis at site of larval penetration
Transient pulmonary symptoms during pulmonary migration of larvae (eosinophilic pneumonitis = Löffler’s syndrome)
Abdominal pain, diarrhea, pruritis ani, larva currens (itchy rash) Hyperinfection: occasional fatal cases caused by massive auto- infection in immunocompromised host; immunoablative therapy, including high-dose corticosteroids, is the most common risk factor for disseminated infection
Treatment
Mebendazole OR albendazole OR pyrantel pamoate
Mebendazole OR albendazole
Ivermectin + doxycycline
Diethylcarbamazine + doxycycline
Diethylcarbamazine
Sticky tape test: eggs adhere to tape applied to perianal skin (need 5-7 tests to rule out) Examination of perianal skin at night may reveal adult worms Usually no eosinophilia as no tissue invasion
Mebendazole, albendazole; pyrantel in pregnancy Change underwear, bathe
in morning, pajamas to bed, wash hands, trim fingernails Treat all family members simultaneously
Reinfection common Ivermectin (OR Albendazole)
3
1. Embryonated eggs ingested by humans 2. Larvae hatch in small intestine
3. Females migrate out anus at night
Figure 15. Life cycle of Enterobius
2
1
3
4
5
6 7
Subtropical, tropical, and temperate (including southern US)
1. Step on stool containing larvae
2. Larvae migrate to lungs via bloodstream
3. Larvae crawl up trachea and down to
GI tract (cough/swallow)
4. Adult worms in intestine
5. Eggs produced in bowel
6. Larvae
7. Bowel movement containing larvae
Figure 16. Life cycle of Strongyloides
© Caillia Matuk © Jenn Platt