Page 765 - TNFlipTest
P. 765
Toronto Notes 2019
Behavioural Neurology
Neurology N23
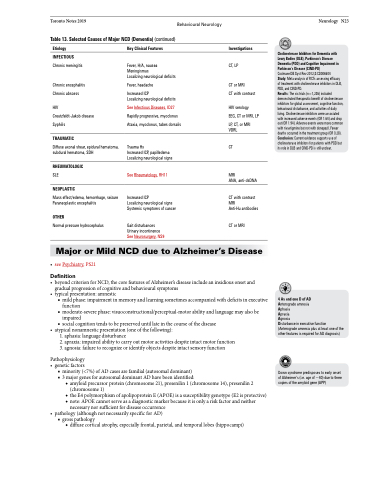
Table 13. Selected Causes of Major NCD (Dementia) (continued)
Etiology
INFECTIOUS
Chronic meningitis
Chronic encephalitis Chronic abscess
HIV
Creutzfeldt-Jakob disease Syphilis
TRAUMATIC
Diffuse axonal shear, epidural hematoma, subdural hematoma, SDH
RHEUMATOLOGIC
SLE
NEOPLASTIC
Mass effect/edema, hemorrhage, seizure Paraneoplastic encephalitis
OTHER
Normal pressure hydrocephalus
Key Clinical Features
Fever, H/A, nausea Meningismus
Localizing neurological deficits
Fever, headache
Increased ICP
Localizing neurological deficits
See Infectious Diseases, ID27
Rapidly progressive, myoclonus Ataxia, myoclonus, tabes dorsalis
Trauma Hx
Increased ICP, papilledema Localizing neurological signs
See Rheumatology, RH11
Increased ICP
Localizing neurological signs Systemic symptoms of cancer
Gait disturbances Urinary incontinence See Neurosurgery, NS9
Investigations
CT, LP
CT or MRI
CT with contrast
HIV serology
EEG, CT or MRI, LP
LP, CT, or MRI VDRL
CT
MRI
ANA, anti-dsDNA
CT with contrast MRI
Anti-Hu antibodies
CT or MRI
Cholinesterase Inhibitors for Dementia with Lewy Bodies (DLB), Parkinson’s Disease Dementia (PDD) and Cognitive Impairment in Parkinson’s Disease (CIND-PD)
Cochrane DB Syst Rev 2012;3:CD006504
Study: Meta-analysis of RCTs assessing efficacy of treatment with cholinesterase inhibitors in DLB, PDD, and CIND-PD.
Results: The six trials (n=1,236) included demonstrated therapeutic benefit of cholinesterase inhibitors for global assessment, cognitive function, behavioural disturbance, and activities of daily living. Cholinesterase inhibitors were associated with increased adverse events (OR 1.64) and drop out (OR 1.94). Adverse events were more common with rivastigmine but not with donepezil. Fewer deaths occurred in the treatment group (OR 0.28). Conclusion: Current evidence supports use of cholinesterase inhibitors for patients with PDD but its role in DLB and CIND-PD is still unclear.
Major or Mild NCD due to Alzheimer’s Disease
• seePsychiatry,PS21
Definition
• beyondcriterionforNCD,thecorefeaturesofAlzheimer’sdiseaseincludeaninsidiousonsetand gradual progression of cognitive and behavioural symptoms
• typicalpresentation:amnestic
■ mild phase: impairment in memory and learning sometimes accompanied with deficits in executive
function
■ moderate-severe phase: visuoconstructional/perceptual-motor ability and language may also be
impaired
■ social cognition tends to be preserved until late in the course of the disease
• atypicalnonamnesticpresentation(oneofthefollowing):
1. aphasia: language disturbance
2. apraxia: impaired ability to carry out motor activities despite intact motor function 3. agnosia: failure to recognize or identify objects despite intact sensory function
Pathophysiology • geneticfactors
■ minority (<7%) of AD cases are familial (autosomal dominant) ■ 3 major genes for autosomal dominant AD have been identified:
◆ amyloid precursor protein (chromosome 21), presenilin 1 (chromosome 14), presenilin 2 (chromosome 1)
◆ the E4 polymorphism of apolipoprotein E (APOE) is a susceptibility genotype (E2 is protective)
◆ note: APOE cannot serve as a diagnostic marker because it is only a risk factor and neither
necessary nor sufficient for disease occurrence • pathology(althoughnotnecessarilyspecificforAD)
■ gross pathology
◆ diffuse cortical atrophy, especially frontal, parietal, and temporal lobes (hippocampi)
4AsandoneDofAD Anterograde amnesia Aphasia
Apraxia
Agnosia
Disturbance in executive function (Anterograde amnesia plus at least one of the other features is required for AD diagnosis)
Down syndrome predisposes to early onset of Alzheimer’s (i.e. age of ~40) due to three copies of the amyloid gene (APP)