Page 95 - TNFlipTest
P. 95
Toronto Notes 2019 Ischemic Heart Disease
6. ACE Inhibitors (ACEI, not used to treat symptomatic angina)
■ angina patients tend to have risk factors for CV disease which warrant use of an ACEI (e.g. HTN, DM, proteinuric renal disease, previous MI with LV dysfunction)
■ benefit in all patients at high risk for CV disease (concomitant DM, renal dysfunction, or LV systolic dysfunction)
7. Invasive Strategies
■ revascularization (see Coronary Revascularization, C31 and COURAGE trial sidebar)
VARIANT ANGINA (PRINZMETAL’S ANGINA)
• myocardialischemiasecondarytocoronaryarteryvasospasm,withorwithoutatherosclerosis • uncommonlyassociatedwithinfarctionorLVdysfunction
• typicallyoccursbetweenmidnightand8am,unrelatedtoexercise,relievedbynitrates
• typicallySTelevationonECG
• diagnosedbyprovocativetestingwithergotvasoconstrictors(rarelydone) • treatwithnitratesandCCBs
SYNDROME X
• typicalsymptomsofanginabutnormalangiogram
• mayshowdefinitesignsofischemiawithexercisetesting
• thoughttobeduetoinadequatevasodilatorreserveofcoronaryresistancevessels • betterprognosisthanovertepicardialatherosclerosis
Acute Coronary Syndromes
Definition
• ACSincludesthespectrumofUA,NSTEMI,andSTEMI;thisdistinctionaidsinprovidingthe appropriate therapeutic intervention
■ MI is defined by evidence of myocardial necrosis. It is diagnosed by a rise/fall of serum markers plus any one of:
◆ symptoms of ischemia (chest/upper extremity/mandibular/epigastric discomfort; dyspnea) ◆ ECG changes (ST-T changes, new BBB or pathological Q waves)
◆ imaging evidence (myocardial loss of viability, wall motion abnormality, or intracoronary
thrombus)
◆ if biomarker changes are unattainable, cardiac symptoms combined with new ECG changes is
sufficient
■ NSTEMImeetscriteriaforMIwithoutSTelevationorBBB
■ STEMImeetscriteriaforMIcharacterizedbySTelevationornewBBB
• UAisclinicallydefinedbyanyofthefollowing:
■ accelerating pattern of pain: increased frequency, increased duration, decreased threshold of
exertion, decreased response to treatment
■ angina at rest
■ new-onset angina
■ angina post-MI or post-procedure (e.g. percutaneous coronary intervention [PCI], coronary artery
bypass grafting [CABG])
Investigations
• historyandphysical
■ note that up to 30% of MIs are unrecognized or “silent” due to atypical symptoms – more common
in women, DM, elderly, post-heart transplant (because of denervation) • ECG
• CXR • labs
■ serum cardiac biomarkers for myocardial damage (repeat 8 h later) (see Cardiac Biomarkers, C11) ■ CBC, INR/PTT, electrolytes and magnesium, creatinine, urea, glucose, serum lipids
■ draw serum lipids within 24-48 h because values are unreliable from 2-48 d post-MI
MANAGEMENT OF ACUTE CORONARY SYNDROMES
1. General Measures
■ ABCs: assess and correct hemodynamic status first ■ bed rest, cardiac monitoring, oxygen
■ nitroglycerin SL followed by IV
■ morphine IV
Cardiology and Cardiac Surgery C27
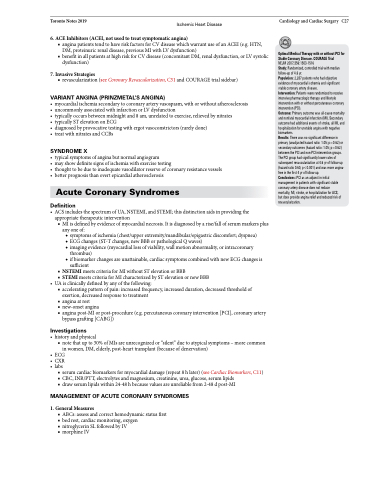
Optimal Medical Therapy with or without PCI for Stable Coronary Disease. COURAGE Trial
NEJM 2007;356:1503-1516
Study: Randomized, controlled trial with median follow-up of 4.6 yr.
Population: 2,287 patients who had objective evidence of myocardial ischemia and significant stable coronary artery disease.
Intervention: Patients were randomized to receive intensive pharmacologic therapy and lifestyle intervention with or without percutaneous coronary intervention (PCI).
Outcome: Primary outcome was all-cause mortality and nonfatal myocardial infarction (MI). Secondary outcome had additional events of stroke, all MI, and hospitalization for unstable angina with negative biomarkers.
Results: There was no significant difference in primary (unadjusted hazard ratio: 1.05; p=0.62) or secondary outcomes (hazard ratio: 1.05; p=0.62) between the PCI and non-PCI intervention groups. The PCI group had significantly lower rates of subsequent revascularization at 4.6 yr of follow-up (hazard ratio 0.60, p<0.001) and was more angina- free in the first 4 yr of follow-up.
Conclusions: PCI as an adjunct in initial management in patients with significant stable coronary artery disease does not reduce mortality, MI, stroke, or hospitalization for ACS, but does provide angina relief and reduced risk of revascularization.