Page 1053 - TNFlipTest
P. 1053
Toronto Notes 2019 Cardiology Cyanotic Congenital Heart Disease
• systemicvenousreturnre-enterssystemiccirculationdirectly
• most prominent feature is cyanosis (O2 sat <75%)
• hyperoxictestdifferentiatesbetweencardiacandothercausesofcyanosis
■ obtain preductal, right radial ABG in room air, then repeat after the child inspires 100% O2
■ if PaO2 improves to greater than 150 mmHg, cyanosis less likely cardiac in origin • pre-ductalandpost-ductalpulseoximetry
■ >5% difference suggests R to L shunt
1 . RIGHT-TO-LEFT SHUNT LESIONS
Tetralogy of Fallot
• epidemiology:10%ofallCHD,mostcommoncyanoticheartdefectdiagnosedbeyondinfancywith peak incidence at 2-4 mo of age
• pathophysiology
■ embryological defect due to anterior and superior deviation of the outlet septum leading to: VSD,
RVOTO (i.e. pulmonary stenosis ± subpulmonary valve stenosis), over-riding aorta, and RVH ◆ infants may initially have a L → R shunt (therefore no cyanosis); however, RVOTO is
progressive, leading to increasing R → L shunting with hypoxemia and cyanosis
◆ degree of RVOTO determines the direction and degree of shunt and, therefore, the extent of
clinical cyanosis and degree of RVH
• clinicalpresentation
■ history: hypoxic “tet” spells
◆ during exertional states (crying, exercise) the increasing pulmonary vascular resistance and
decrease in systemic resistance causes an increase in right-to-left shunting
◆ clinical features include paroxysms of rapid and deep breathing, irritability and crying,
increasing cyanosis, decreased intensity of murmur (decreased flow across RVOTO), patient
squatting for relief (increased peripheral resistance, decreased R to L shunting) ◆ if severe, can lead to decreased level of consciousness, seizures, death
■ physical exam
◆ single loud S2 due to severe pulmonary stenosis (i.e. RVOTO), SEM at LSB
• investigations
■ ECG: RAD, RVH
■ CXR: boot-shaped heart, decreased pulmonary vasculature, right aortic arch (in 20%) ■ Echo: diagnostic
• managementofspells:O2,knee-chestposition,fluidbolus,morphinesulfate,propranolol
• treatment:surgicalrepairat4-6moofage;earlierifmarkedcyanosisor“tet”spells
2 . OTHER CYANOTIC CONGENITAL HEART DISEASES
Transposition of the Great Arteries (TGA)
• epidemiology:3-5%ofallcongenitalcardiaclesions,mostcommoncyanoticCHDinneonates • pathophysiology:parallelpulmonaryandsystemiccirculations
■ systemic:body→RA→RV→aorta→body
■ pulmonary:lungs→LA→LV→pulmonaryartery→lungs ■ survival is dependent on mixing through PDA, ASD, or VSD
• physicalexam
■ neonates:ductusarteriosusclosurecausesrapidlyprogressiveseverehypoxemiaunresponsiveto
oxygen therapy, acidosis, and death
■ VSD present: cyanosis is not prominent; CHF within first weeks of life ■ VSD absent: no murmur
• investigations
■ ECG: RAD, RVH, or may be normal
■ CXR: egg-shaped heart with narrow mediastinum (“egg on a string”) ■ Echo: diagnostic
• management
■ symptomatic neonates: prostaglandin E1 infusion to keep ductus open until balloon atrial
septostomy
■ surgical repair: arterial switch performed in the first two weeks in those without a VSD while LV
muscle is still strong
Total Anomalous Pulmonary Venous Return
• epidemiology:1-2%ofCHD • pathophysiology
■ all pulmonary veins drain into right-sided circulation (systemic veins, RA)
■ no direct oxygenated pulmonary venous return to left atrium
■ often associated with obstruction at connection sites
■ ASD must be present for oxygenated blood to shunt into the LA and systemic circulation
• management:surgicalrepairinallcasesandrequiredurgentlyforseverecyanosis
Pediatrics P19
Causes of Cyanotic Heart Disease – 5T’s Truncus arteriosus
Transposition of the great vessels Tricuspid atresia
Tetralogy of Fallot
Total anomalous pulmonary venous return
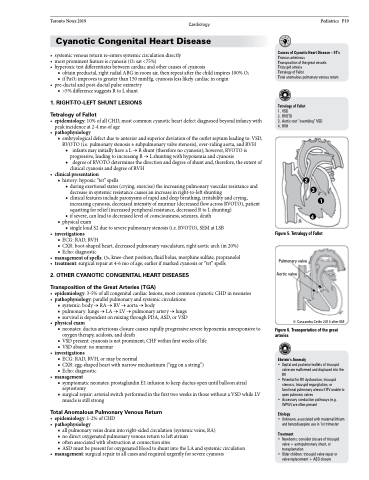
Tetralogy of Fallot
1. VSD
2. RVOTO
3. Aortic root “overriding” VSD 4. RVH
2
Figure5.TetralogyofFallot
Pulmonary valve Aortic valve
© Cassandra Cetlin 2014 after KM
Figure6.Transportationofthegreat arteries
Ebstein’s Anomaly
• Septal and posterior leaflets of tricuspid valve are malformed and displaced into the RV
• Potential for RV dysfunction, tricuspid stenosis, tricuspid regurgitation, or functional pulmonary atresia if RV unable to open pulmonic valves
• Accessory conduction pathways (e.g. WPW) are often present
Etiology
• Unknown, associated with maternal lithium and benzodiazepine use in 1st trimester
Treatment
• Newborns: consider closure of tricuspid valve + aortopulmonary shunt, or transplantation
• Older children: tricuspid valve repair or valve replacement + ASD closure
3
1
4