Page 1291 - TNFlipTest
P. 1291
Toronto Notes 2019 Septic Arthritis Septic Arthritis
• septicarthritisisamedicalemergency,itcanleadtorapidjointdestructionandhasa10-15%riskof mortality
• knee and hip are most commonly affected joints, with knee accounting for approximately 50% of cases
• mostcommonlycausedbyhematogenousspreadofbacterialinfection(grampositivecocci>gram
negative bacilli)
• riskfactors:veryyoungorveryoldage(>80),portalofentry(IVdruguse),recentinfection,RA
(related to prior joint damage and immunosuppressed state of host), type 2 DM
• poorprognosticfactors:olderage,immunocompromised,delayintreatment,previouslydamagedjoint,
joint prosthesis
• considerempiricantibiotictherapyuntilsepticarthritisisexcludedfromhistory,physicalexamination,
and synovial fluid analysis
• seeInfectiousDiseases,ID14andOrthopedics,SpeticJointOR11 Degenerative Arthritis: Osteoarthritis
• seeFamilyMedicine,FM40
Definition
• progressivedeteriorationofarticularcartilageandsurroundingjointstructurescausedbygenetic, metabolic, biochemical, and biomechanical factors with secondary components of inflammation
Classification (Based on Etiology)
• primary(idiopathic)
■ most common, unknown etiology
• secondary
■ post-traumatic or mechanical
■ post-inflammatory (e.g. RA) or post-infectious
■ heritable skeletal disorders (e.g. scoliosis)
■ endocrine disorders (e.g. acromegaly, hyperparathyroidism, hypothyroidism)
■ metabolic disorders (e.g. gout, pseudogout, hemochromatosis, Wilson’s disease, ochronosis) ■ neuropathic (e.g. Charcot joints)
◆ atypical joint trauma due to peripheral neuropathy (e.g. DM, syphilis) ■ avascular necrosis (AVN)
■ other (e.g. congenital malformation)
Pathophysiology
• theprocessappearstobeinitiatedbyabnormalitiesinbiomechanicalforcesand/or,lessoften,in cartilage
• elevatedproductionofpro-inflammatorycytokinesisimportantinOAprogression
• tissuecatabolism>repair
• contributingfactors(mechanismsunknown):genetics,alignment(bow-legged,knock-kneed),joint
deformity (hip dysplasia), joint injury (meniscal or ligament tears), obesity, environmental, mechanical
loading, age, and gender
• nowconsideredtobeasystemicmusculoskeletaldisorderratherthanafocaldisorderofsynovialjoints
Epidemiology
• mostcommonarthropathy(accountsfor~75%ofallarthritis)
• increasedprevalencewithincreasingage(35%of30yrolds,85%of80yrolds)
Risk Factors
• geneticpredisposition,advancedage,obesity(forkneeandhandOA),female,trauma
Rheumatology RH5
Septic arthritis is a medical emergency; it leads to rapid joint destruction, and there is a 10-15% risk of mortality
OA of MCP joints can be seen in hemochromatosis or CPPD-related disease (chondrocalcinosis)
ESR can also be elevated in anemia, end- stage renal disease, females, increased age, and obesity
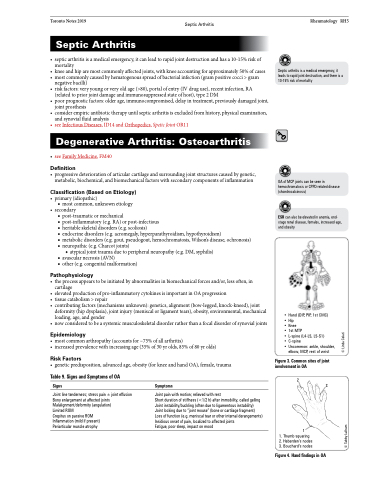
Table 9. Signs and Symptoms of OA
Signs
Joint line tenderness; stress pain ± joint effusion Bony enlargement at affected joints Malalignment/deformity (angulation)
Limited ROM
Crepitus on passive ROM Inflammation (mild if present) Periarticular muscle atrophy
Symptoms
Joint pain with motion; relieved with rest
Short duration of stiffness (<1/2 h) after immobility, called gelling Joint instability/buckling (often due to ligamentous instability) Joint locking due to “joint mouse” (bone or cartilage fragment) Loss of function (e.g. meniscal tear or other internal derangements) Insidious onset of pain, localized to affected joints
Fatigue, poor sleep, impact on mood
2
1
1. Thumb squaring
2. Heberden’s nodes 3. Bouchard’s nodes
3
• Hand (DIP, PIP, 1st CMC) • Hip
• Knee
• 1st MTP
• L-spine (L4-L5, L5-S1)
• C-spine
• Uncommon: ankle, shoulder,
elbow, MCP, rest of wrist
Figure 3. Common sites of joint involvement in OA
Figure 4. Hand findings in OA
© Tabby Lulham
© Linda Colati