Page 1289 - TNFlipTest
P. 1289
Toronto Notes 2019
Differential Diagnoses of Common Presentations
Rheumatology RH3
Table 2. Classes of MHCs
MHC Class
I II III
Types
HLA-A, B, C HLA-DP, DQ, DR
Some components of the complement cascade
Location
All cells
Ag presenting cells (mononuclear phagocytes, B cells, etc.)
In plasma
Comments
Function
Recognized by CD8+ (cytotoxic) T-lymphocytes
Recognized by CD4+ (helper) T-lymphocytes
Chemotaxis, opsonization, lysis of bacteria and cells
Adaptive Immune Cells
• B-cell: produce antibodies after activation
by specific antigen and B-cell co-receptor, additional signals provided by CD4 T helper cells
• Cytotoxic T-cell: CD8, direct cytotoxicity of target cells at sites of infection, kill via lytic granules and FasL-Fas interaction, recognize specific antigen and MHC1
• Helper T-cell: subset of CD4 cells, activate and help other types of cells carry out immune defense (activate macrophages, help B cells, release cytokines)
• Regulatory T-cell: subset of CD4 cells, suppress activation of naïve autoreactive T cells
Table 3. HLA-Associated Rheumatic Disease
HLA Type
B27
DR4, DR1 DR3
Associated Conditions
Ankylosing Spondylitis (AS) Reactive Arthritis (ReA) Enteropathic arthritis (EA)
Rheumatoid Arthritis (RA)
Sjögren’s syndrome (SS)
Systemic Lupus Erythematosus (SLE)
Relative risk 20x for developing AS and ReA
In RA, relative risk = 2-10x; found in 93% of patients
DR3 is associated with the production of anti-Ro/SSA and anti- La/SSB antibodies
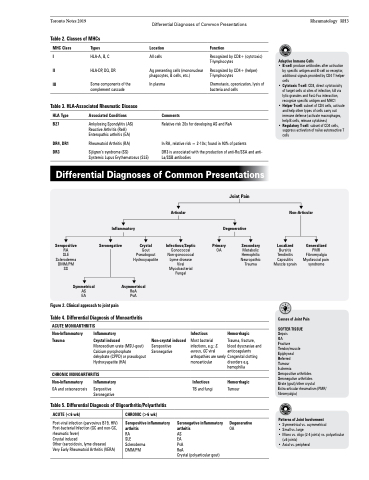
Differential Diagnoses of Common Presentations
Articular
Infectious/Septic
Gonococcal Non-gonococcal Lyme disease Viral Mycobacterial Fungal
Joint Pain
Degenerative
Non-Articular
Inflammatory Seronegative
Crystal
Primary
OA
Secondary
Metabolic Hemophilic Neuropathic Trauma
Hemorrhagic
Trauma, fracture, blood dyscrasias and anticoagulants Congenital clotting disorders e.g. hemophilia
Hemorrhagic
Tumour
Degenerative
OA
Localized
Bursitis Tendinitis Capsulitis Muscle sprain
Generalized
PMR Fibromyalgia Myofascial pain syndrome
Seropositive
RA
SLE Scleroderma DMM/PM SS
Symmetrical
AS EA
Figure 2. Clinical approach to joint pain
Gout Pseudogout Hydroxyapatite
Asymmetrical
ReA PsA
Table 4. Differential Diagnosis of Monoarthritis
ACUTE MONOARTHRITIS
Causes of Joint Pain SOFTER TISSUE
Sepsis
OA
Fracture
Tendon/muscle
Epiphyseal
Referred
Tumour
Ischemia
Seropositive arthritides Seronegative arthritides
Urate (gout)/other crystal Extra-articular rheumatism (PMR/ fibromyalgia)
Patterns of Joint Involvement
• Symmetrical vs. asymmetrical
• Small vs. large
• Mono vs. oligo (2-4 joints) vs. polyarticular
(≥5 joints)
• Axial vs. peripheral
Non-Inflammatory Trauma
Inflammatory Crystal induced
Monosodium urate (MSU-gout) Calcium pyrophosphate dehydrate (CPPD) or pseudogout Hydroxyapatite (HA)
Infectious
Non-Inflammatory
OA and osteonecrosis
Inflammatory
Serpositive Seronegative
Non-crystal induced
Seropositive Seronegative
Most bacterial infections, e.g.: S. aureus, GC viral arthopathies are rarely monoarticular
Infectious
TB and fungi
Seronegative inflammatory arthritis
AS
EA
PsA
ReA
Crystal (polyarticular gout)
CHRONIC MONOARTHRITIS
Table 5. Differential Diagnosis of Oligoarthritis/Polyarthritis
ACUTE (<6 wk)
Post-viral infection (parvovirus B19, HIV) Post-bacterial Infection (GC and non-GC, rheumatic fever)
Crystal induced
Other (sarcoidosis, lyme disease)
Very Early Rheumatoid Arthritis (VERA)
CHRONIC (>6 wk)
Seropositive inflammatory arthritis
RA
SLE
Scleroderma DMM/PM