Page 182 - TNFlipTest
P. 182
ER2 Emergency Medicine
Acronyms
Toronto Notes 2019
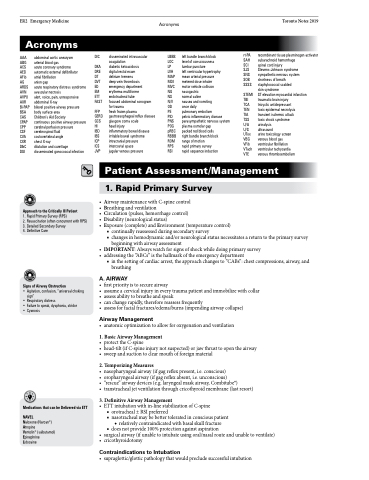
Acronyms
AAA abdominal aortic aneurysm ABG arterial blood gas
ACS acute coronary syndrome AED automatic external defibrillator AFib atrial fibrillation
AG anion gap
ARDS acute respiratory distress syndrome AVN avascular necrosis
AVPU alert, voice, pain, unresponsive AXR abdominal X-ray
Bi-PAP bilevel positive airway pressure BSA body surface area
CAS Children’s Aid Society
CPAP continuous positive airway pressure CPP cerebral perfusion pressure
CSF cerebrospinal fluid
CVA costovertebral angle
CXR chest X-ray
D&C dilatation and curettage
DGI disseminated gonococcal infection
Approach to the Critically Ill Patient
1. Rapid Primary Survey (RPS)
2. Resuscitation (often concurrent with RPS) 3. Detailed Secondary Survey
4. Definitive Care
Signs of Airway Obstruction
• Agitation, confusion, “universal choking sign”
• Respiratory distress
• Failure to speak, dysphonia, stridor
• Cyanosis
DIC disseminated intravascular coagulation
DKA diabetic ketoacidosis
DRE digital rectal exam
DT delirium tremens
DVT deep vein thrombosis
ED emergency department
EM erythema multiforme
ETT endotracheal tube
FAST focused abdominal sonogram
for trauma
FFP fresh frozen plasma
GERD gastroesophageal reflux disease GCS glasgow coma scale
HI head injury
IBD inflammatory bowel disease IBS irritable bowel syndrome
ICP intracranial pressure ICS intercostal space
JVP jugular venous pressure
LBBB left bundle branch block LOC level of consciousness
LP lumbar puncture
LVH left ventricular hypertrophy MAP mean arterial pressure MDI metered dose inhaler
MVC motor vehicle collision NG nasogastric
NS normal saline
N/V nausea and vomiting OD once daily
PE pulmonary embolism
PID pelvic inflammatory disease
PNS parasympathetic nervous system POG plasma osmolar gap
pRBC packed red blood cells
RBBB right bundle branch block
ROM range of motion
RPS rapid primary survey
RSI rapid sequence induction
rt-PA recombinant tissue plasminogen activator SAH subarachnoid hemorrhage
SCI spinal cord injury
SJS Stevens-Johnson syndrome
SNS sympathetic nervous system SOB shortness of breath
SSSS staphylococcal scalded
skin syndrome
STEMI ST elevation myocardial infarction TBI traumatic brain injury
TCA tricyclic antidepressant
TEN toxic epidermal necrolysis
TIA transient ischemic attack
TSS toxic shock syndrome
U/A urinalysis
U/S ultrasound
UTox urine toxicology screen
VBG venous blood gas
VFib ventricular fibrillation
VTach ventricular tachycardia
VTE venous thromboembolism
Medications that can be Delivered via ETT
NAVEL
Naloxone (Narcan®) Atropine
Ventolin® (salbutamol) Epinephrine
Lidocaine
Patient Assessment/Management
1. Rapid Primary Survey
• AirwaymaintenancewithC-spinecontrol • Breathingandventilation
• Circulation(pulses,hemorrhagecontrol) • Disability(neurologicalstatus)
• Exposure(complete)andEnvironment(temperaturecontrol)
■ continually reassessed during secondary survey
■ changes in hemodynamic and/or neurological status necessitates a return to the primary survey
beginning with airway assessment
• IMPORTANT:Alwayswatchforsignsofshockwhiledoingprimarysurvey • addressingthe“ABCs”isthehallmarkoftheemergencydepartment
■ in the setting of cardiac arrest, the approach changes to “CABs”: chest compressions, airway, and breathing
A . AIRWAY
• firstpriorityistosecureairway
• assumeacervicalinjuryineverytraumapatientandimmobilizewithcollar • assessabilitytobreatheandspeak
• canchangerapidly,thereforereassessfrequently
• assessforfacialfractures/edema/burns(impendingairwaycollapse)
Airway Management
• anatomicoptimizationtoallowforoxygenationandventilation
1. Basic Airway Management
• protecttheC-spine
• head-tilt(ifC-spineinjurynotsuspected)orjawthrusttoopentheairway • sweepandsuctiontoclearmouthofforeignmaterial
2. Temporizing Measures
• nasopharyngealairway(ifgagreflexpresent,i.e.conscious)
• oropharyngealairway(ifgagreflexabsent,i.e.unconscious)
• “rescue”airwaydevices(e.g.laryngealmaskairway,Combitube®)
• transtrachealjetventilationthroughcricothyroidmembrane(lastresort)
3. Definitive Airway Management
• ETTintubationwithin-linestabilizationofC-spine
■ orotracheal ± RSI preferred
■ nasotracheal may be better tolerated in conscious patient
◆ relatively contraindicated with basal skull fracture ■ does not provide 100% protection against aspiration
• surgicalairway(ifunabletointubateusingoral/nasalrouteandunabletoventilate) • cricothyroidotomy
Contraindications to Intubation
• supraglottic/glotticpathologythatwouldprecludesuccessfulintubation