Page 183 - TNFlipTest
P. 183
Toronto Notes 2019
Patient Assessment/Management
Emergency Medicine ER3
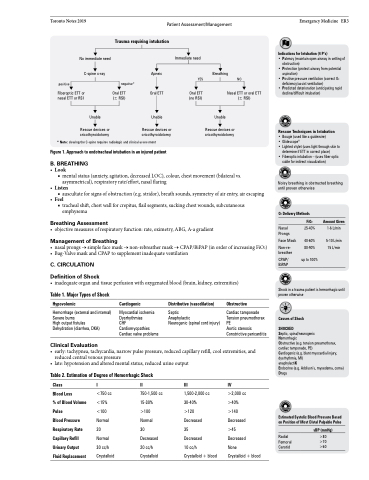
No immediate need C-spine x-ray
Apneic Oral ETT
Unable
Rescue devices or cricothyroidotomy
Immediate need
YES
Oral ETT (no RSI)
Breathing
Nasal ETT or oral ETT (± RSI)
Unable
Rescue devices or cricothyroidotomy
Indications for Intubation (4 P’s)
• Patency (maintain open airway in setting of
obstruction)
• Protection (protect airway from potential
aspiration)
• Positive pressure ventilation (correct O2
deficiency/assist ventilation)
• Predicted deterioration (anticipating rapid
decline/difficult intubation)
Rescue Techniques in Intubation
• Bougie (used like a guidewire)
• Glidescope®
• Lighted stylet (uses light through skin to
determine if ETT in correct place)
• Fiberoptic intubation – (uses fiber optic
cable for indirect visualization)
Noisy breathing is obstructed breathing until proven otherwise
Trauma requiring intubation
NO
positive
negative*
Oral ETT (± RSI)
Fiberoptic ETT or nasal ETT or RSI
Unable
Rescue devices or cricothyroidotomy
* Note: clearing the C-spine requires radiologic and clinical assessment Figure 1. Approach to endotracheal intubation in an injured patient
B . BREATHING
• Look
■ mental status (anxiety, agitation, decreased LOC), colour, chest movement (bilateral vs.
asymmetrical), respiratory rate/effort, nasal flaring • Listen
■ auscultate for signs of obstruction (e.g. stridor), breath sounds, symmetry of air entry, air escaping • Feel
■ tracheal shift, chest wall for crepitus, flail segments, sucking chest wounds, subcutaneous emphysema
Breathing Assessment
• objectivemeasuresofrespiratoryfunction:rate,oximetry,ABG,A-agradient
Management of Breathing
• nasalprongs→simplefacemask→non-rebreathermask→CPAP/BiPAP(inorderofincreasingFiO2) • Bag-ValvemaskandCPAPtosupplementinadequateventilation
C . CIRCULATION Definition of Shock
• inadequateorganandtissueperfusionwithoxygenatedblood(brain,kidney,extremities)
O2 Delivery Methods
Nasal Prongs
Face Mask
Non-re- breather
CPAP/ BiPAP
FiO2
25-40%
40-60% 80-90%
up to 100%
Amount Given
1-6 L/min
5-10 L/min 15 L/min
Table 1. Major Types of Shock
Hypovolemic
Hemorrhage (external and internal) Severe burns
High output fistulas
Dehydration (diarrhea, DKA)
Clinical Evaluation
Cardiogenic
Myocardial ischemia Dysrhythmias
CHF
Cardiomyopathies Cardiac valve problems
Distributive (vasodilation)
Septic
Anaphylactic
Neurogenic (spinal cord injury)
Obstructive
Cardiac tamponade Tension pneumothorax PE
Aortic stenosis Constrictive pericarditis
Shock in a trauma patient is hemorrhagic until proven otherwise
Causes of Shock
SHOCKED
Septic, spinal/neurogenic
Hemorrhagic
Obstructive (e.g. tension pneumothorax, cardiac tamponade, PE)
Cardiogenic (e.g. blunt myocardial injury, dysrhythmia, MI)
anaphylactiK
Endocrine (e.g. Addison’s, myxedema, coma) Drugs
Estimated Systolic Blood Pressure Based on Position of Most Distal Palpable Pulse
• early:tachypnea,tachycardia,narrowpulsepressure,reducedcapillaryrefill,coolextremities,and reduced central venous pressure
• late:hypotensionandalteredmentalstatus,reducedurineoutput
Table 2. Estimation of Degree of Hemorrhagic Shock
Class
Blood Loss
% of Blood Volume Pulse
Blood Pressure Respiratory Rate Capillary Refill Urinary Output Fluid Replacement
I
<750 cc <15% <100 Normal 20 Normal 30 cc/h Crystalloid
II
750-1,500 cc 15-30% >100 Normal
30 Decreased 20 cc/h Crystalloid
III
1,500-2,000 cc 30-40%
>120 Decreased
35
Decreased
10 cc/h
Crystalloid + blood
IV
>2,000 cc
>40%
>140
Decreased
>45
Decreased
None
Crystalloid + blood
Radial Femoral Carotid
sBP (mmHg)
>80 >70 >60