Page 190 - TNFlipTest
P. 190
ER10 Emergency Medicine
Traumatology
Toronto Notes 2019
The Canadian C-Spine Rule
JAMA2001;286:1841-48
For Alert (GCS Score = 15) and Stable Trauma
Patients where C-Spine Injury is a Concern
■ indications
◆ C-spineinjury
◆ unconscious patients (with appropriate mechanism of injury) ◆ neurological symptoms or findings
◆ deformities that are palpable when patient is log rolled
◆ back pain
◆ bilateral calcaneal fractures (due to fall from height)
– concurrent burst fractures of the lumbar or thoracic spine in 10% (T11-L2)
◆ consider CT (for subtle bony injuries), MRI (for soft tissue injuries) if appropriate
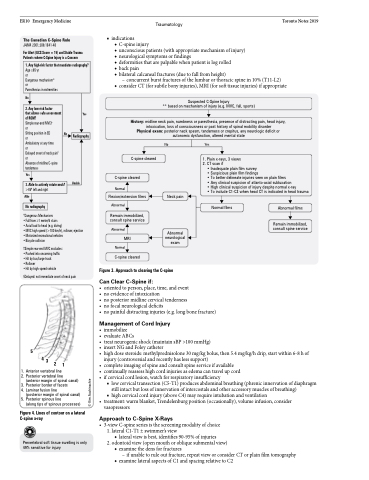
Suspected C-Spine Injury
** based on mechanism of injury (e.g. MVC, fall, sports)
History: midline neck pain, numbness or paresthesia, presence of distracting pain, head injury, intoxication, loss of consciousness or past history of spinal mobility disorder Physical exam: posterior neck spasm, tenderness or crepitus, any neurologic deficit or autonomic dysfunction, altered mental state
1. Any high-risk factor that mandates radiography?
Age ≥65 yr
or
Dangerous mechanism* or
Paresthesias in extremities
No
2. Any low-risk factor
that allows safe assessment of ROM?
Simple rear-end MVC†
or
Sitting position in ED
or
Ambulatory at any time
or
Delayed onset of neck pain§ or
Absence of midline C-spine tenderness
Yes
No
Radiography
Yes
Able
Unable
C-spine cleared
C-spine cleared
Normal Flexion/extension films
Abnormal
Remain immobilized, consult spine service
Abnormal
MRI Normal
C-spine cleared
No
Neck pain
Abnormal neurological exam
Yes
1. Plain x-rays, 3 views 2. CT scan if
• Inadequate plain film survey
• Suspicious plain film findings
• To better delineate injuries seen on plain films
• Any clinical suspicion of atlanto-axial subluxation
• High clinical suspicion of injury despite normal x-ray
• To include C1-C3 when head CT is indicated in head trauma
3. Able to actively rotate neck?
>45o left and right
No radiography
Normal films
Abnormal films
Remain immobilized, consult spine service
*Dangerous Mechanism:
• Fall from ≥1 meter/5 stairs
• Axial load to head (e.g. diving)
• MVC high speed (>100 km/h), rollover, ejection • Motorized recreational vehicles
• Bicycle collision
†Simple rear-end MVC excludes: • Pushed into oncoming traffic • Hit by bus/large truck
• Rollover
• Hit by high-speed vehicle
§Delayed: not immediate onset of neck pain
5
1
1. Anterior vertebral line
2. Posterior vertebral line
(anterior margin of spinal canal)
3. Posterior border of facets
4. Laminar fusion line
(posterior margin of spinal canal)
5. Posterior spinous line
(along tips of spinous processes)
Figure 4. Lines of contour on a lateral C-spine x-ray
Prevertebral soft tissue swelling is only 49% sensitive for injury
Figure 3. Approach to clearing the C-spine
Can Clear C-Spine if:
• orientedtoperson,place,time,andevent • noevidenceofintoxication
• noposteriormidlinecervicaltenderness • nofocalneurologicaldeficits
432
• immobilize
• evaluateABCs
• treatneurogenicshock(maintainsBP>100mmHg)
• insertNGandFoleycatheter
• highdosesteroids:methylprednisolone30mg/kgbolus,then5.4mg/kg/hdrip,startwithin6-8hof
injury (controversial and recently has less support)
• complete imaging of spine and consult spine service if available
• continually reassess high cord injuries as edema can travel up cord • ifcervicalcordlesion,watchforrespiratoryinsufficiency
■ low cervical transection (C5-T1) produces abdominal breathing (phrenic innervation of diaphragm still intact but loss of innervation of intercostals and other accessory muscles of breathing)
■ high cervical cord injury (above C4) may require intubation and ventilation
• treatment:warmblanket,Trendelenburgposition(occasionally),volumeinfusion,consider
vasopressors
Approach to C-Spine X-Rays
• 3-viewC-spineseriesisthescreeningmodalityofchoice 1. lateral C1-T1 ± swimmer’s view
◆ lateral view is best, identifies 90-95% of injuries
2. odontoid view (open mouth or oblique submental view)
◆ examine the dens for fractures
– if unable to rule out fracture, repeat view or consider CT or plain film tomography
◆ examine lateral aspects of C1 and spacing relative to C2
• nopainfuldistractinginjuries(e.g.longbonefracture)
Management of Cord Injury
© Kim Auchinachie