Page 527 - TNFlipTest
P. 527
Toronto Notes 2019 Gynecological Oncology
• generallyslowgrowing,excellentprognosis
■ 5 yr survival >99%
■ recurrences tend to occur late, may be associated with low grade serous carcinoma
Gynecology GY41
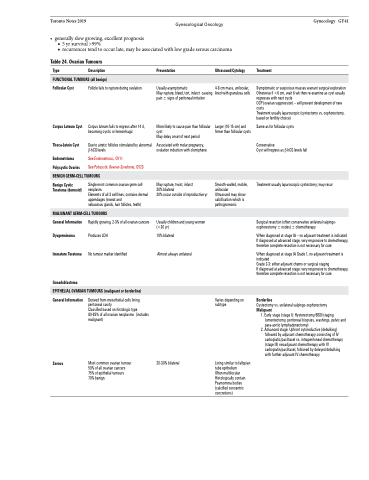
Table 24. Ovarian Tumours
Type Description
FUNCTIONAL TUMOURS (all benign)
Presentation
Usually asymptomatic Mayrupture,bleed,tort,infarct causing pain ± signs of peritoneal irritation
More likely to cause pain than follicular cyst
May delay onset of next period
Associated with molar pregnancy, ovulation induction with clomiphene
May rupture, twist, infarct
20% bilateral
20% occur outside of reproductive yr
Usually children and young women (<30 yr)
10% bilateral
Almost always unilateral
Ultrasound/Cytology
4-8 cm mass, unilocular, linedwithgranulosacells
Larger (10-15 cm) and firmer than follicular cysts
Smooth-walled, mobile, unilocular
Ultrasound may show calcification which is pathognomonic
Treatment
Symptomatic or suspicious masses warrant surgical exploration Otherwiseif<6cm,wait6wkthenre-examineascystusually regresses with next cycle
OCP (ovarian suppression) – will prevent development of new cysts
Treatment usually laparoscopic (cystectomy vs. oophorectomy, based on fertility choice)
Same as for follicular cysts Conservative
Cyst will regress as β-hCG levels fall
Treatment usually laparoscopic cystectomy; may recur
Surgical resection (often conservative unilateral salpingo- oophorectomy ± nodes) ± chemotherapy
When diagnosed at stage IA – no adjuvant treatment is indicated If diagnosed at advanced stage, very responsive to chemotherapy, therefore complete resection is not necessary for cure
When diagnosed at stage IA Grade 1, no adjuvant treatment is indicated
Grade 2-3: either adjuvant chemo or surgical staging
If diagnosed at advanced stage: very responsive to chemotherapy, therefore complete resection is not necessary for cure
Borderline
Cystectomy vs. unilateral salpingo-oophorectomy
Malignant
1. Early stage (stage I): Hysterectomy/BSO/staging (omentectomy, peritoneal biopsies, washings, pelvic and para-aortic lymphadenectomy)
2. Advanced stage: Upfront cytoreductive (debulking) followed by adjuvant chemotherapy consisting of IV carboplatic/paclitaxel vs. intraperitoneal chemotherapy (stage III) neoadjuvant chemotherapy with IV carboplatin/paclitaxel, followed by delayed debulking with further adjuvant IV chemotherapy
Follicular Cyst
Corpus Luteum Cyst
Theca-Lutein Cyst
Endometrioma Polycystic Ovaries
Benign Cystic Teratoma (dermoid)
General Information Dysgerminoma
Immature Teratoma
Gonadoblastoma
Follicle fails to rupture during ovulation
Corpus luteum fails to regress after 14 d, becoming cystic or hemorrhagic
Due to atretic follicles stimulated by abnormal β-hCG levels
See Endometriosis, GY11
See Polycystic Ovarian Syndrome, GY23
Single most common ovarian germ cell neoplasm
Elements of all 3 cell lines; contains dermal appendages (sweat and
sebaceous glands, hair follicles, teeth)
Rapidly growing, 2-3% of all ovarian cancers Produces LDH
No tumour marker identified
BENIGN GERM-CELL TUMOURS
MALIGNANT GERM-CELL TUMOURS
EPITHELIAL OVARIAN TUMOURS (malignant or borderline)
General Information
Serous
Derived from mesothelial cells lining peritoneal cavity
Classified based on histologic type 80-85% of all ovarian neoplasms (includes malignant)
Most common ovarian tumour 50% of all ovarian cancers 75% of epithelial tumours 70% benign
20-30% bilateral
Varies depending on subtype
Lining similar to fallopian tube epithelium
Often multilocular Histologically contain Psamomma bodies (calcified concentric concretions)