Page 712 - TNFlipTest
P. 712
NP12 Nephrology
• Hypokalemia often accompanied by metabolic alkalosis
• Potassium leaves cells, replaced by H+
• Kidney tubular cells see high H+, think acidosis, and increase ammonium
synthesis and excretion
• Increase in bicarbonate generation
Electrolyte Disorders Toronto Notes 2019 1234
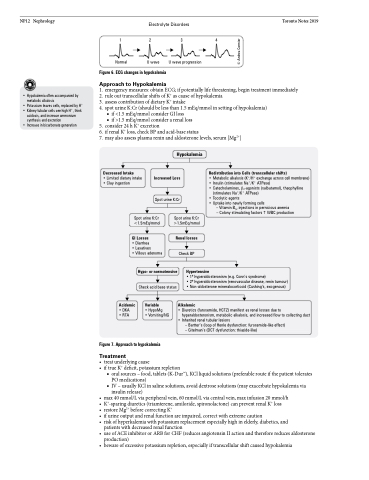
Normal U wave U wave progression
Figure 6. ECG changes in hypokalemia
Approach to Hypokalemia
1. emergency measures: obtain ECG; if potentially life threatening, begin treatment immediately 2. rule out transcellular shifts of K+ as cause of hypokalemia
3. assess contribution of dietary K+ intake
4. spot urine K:Cr (should be less than 1.5 mEq/mmol in setting of hypokalemia)
■ if <1.5 mEq/mmol consider GI loss
■ if >1.5 mEq/mmol consider a renal loss
5. consider 24 h K+ excretion
6. if renal K+ loss, check BP and acid-base status
7. may also assess plasma renin and aldosterone levels, serum [Mg2+]
Decreased Intake
• Limited dietary intake • Clay ingestion
Hypokalemia
Increased Loss
Spot urine K:Cr
Redistribution into Cells (transcellular shifts)
• Metabolic alkalosis (K+/H+ exchange across cell membrane) • Insulin (stimulates Na+/K+ ATPase)
• Catecholamines, β2-agonists (salbutamol), theophylline
(stimulates Na+/K+ ATPase)
• Tocolytic agents
• Uptake into newly forming cells
– Vitamin B12 injections in pernicious anemia
– Colony stimulating factorsWBC production
Spot urine K:Cr <1.5mEq/mmol
GI Losses
• Diarrhea
• Laxatives
• Villous adenoma
Spot urine K:Cr >1.5mEq/mmol
Renal losses
Check BP
Hypertensive
Acidemic
• DKA • RTA
Hypo- or normotensive
Check acid base status
Variable
• HypoMg
• Vomiting/NG
• 1o hyperaldosteronism (e.g. Conn’s syndrome)
• 2o hyperaldosteronism (renovascular disease, renin tumour) • Non-aldosterone mineralocorticoid (Cushing’s, exogenous)
Alkalemic
• Diuretics (furosemide, HCTZ) manifest as renal losses due to hyperaldosteronism, metabolic alkalosis, and increased flow to collecting duct
• Inherited renal tubular lesions
– Bartter’s (loop of Henle dysfunction: furosemide-like effect) – Gitelman’s (DCT dysfunction: thiazide-like)
Figure 7. Approach to hypokalemia
Treatment
• treatunderlyingcause
• if true K+ deficit, potassium repletion
■ oral sources – food, tablets (K-DurTM), KCl liquid solutions (preferable route if the patient tolerates PO medications)
■ IV – usually KCl in saline solutions, avoid dextrose solutions (may exacerbate hypokalemia via insulin release)
• max40mmol/Lviaperipheralvein,60mmol/Lviacentralvein,maxinfusion20mmol/h
• K+-sparing diuretics (triamterene, amiloride, spironolactone) can prevent renal K+ loss
• restore Mg2+ before correcting K+
• ifurineoutputandrenalfunctionareimpaired,correctwithextremecaution
• riskofhyperkalemiawithpotassiumreplacementespeciallyhighinelderly,diabetics,and patients with decreased renal function
• useofACEinhibitororARBforCHF(reducesangiotensinIIactionandthereforereducesaldosterone production)
• bewareofexcessivepotassiumrepletion,especiallyiftranscellularshiftcausedhypokalemia
© Andrea Cormier