Page 98 - TNFlipTest
P. 98
C30 Cardiology and Cardiac Surgery
Ischemic Heart Disease Toronto Notes 2019
6. Angiotensin-Converting Enzyme Inhibitors
■ prevent adverse ventricular remodelling
■ recommended for asymptomatic high-risk patients (e.g. diabetics), even if LVEF >40% ■ recommended for symptomatic CHF, reduced LVEF (<40%), anterior MI
■ use ARBs in patients who are intolerant of ACEI; avoid combining ACE and ARB
7. ± Aldosterone Antagonists
■ if on ACEI and β-blockers and LVEF <40% and CHF or DM ■ significant mortality benefit shown with eplerenone by 30 d
8. Statins (early, intensive, irrespective of cholesterol level; e.g. atorvastatin 80 mg daily) 9. Invasive Cardiac Catheterization if indicated (risk stratification)
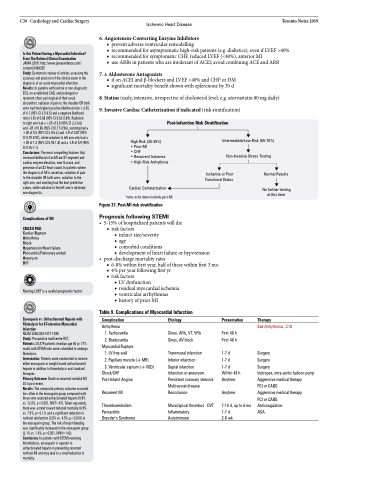
Post-Infarction Risk Stratification
Is this Patient Having a Myocardial Infarction? From The Rational Clinical Examination JAMA 2009; http://www.jamaevidence.com/ content/3484335
Study: Systematic review of articles assessing the accuracy and precision of the clinical exam in the diagnosis of an acute myocardial infarction. Results: In patients with normal or non-diagnostic ECG, no established CAD, and prolonged or recurrent chest pain typical of their usual discomfort, radiation of pain to the shoulder OR both arms had the highest positive likelihood ratio (+LR) of 4.1 (95% CI 2.5-6.5) and a negative likelihood ratio (-LR) of 0.68 (95% CI 0.52-0.89). Radiation
to right arm had a +LR of 3.8 (95% CI 2.2-6.6)
and –LR of 0.86 (95% CI 0.77-0.96), vomiting had a +LR of 3.5 (95% CI 2.0-6.2) and –LR of 0.87 (95% Cl 0.79-0.97), while radiation to left arm only had a +LR of 1.3 (95% CI 0.93-1.8) and a –LR of 0.9 (95% CI 0.76-1.1).
Conclusions: The most compelling features that increase likelihood of an MI are ST-segment and cardiac enzyme elevation, new Q-wave, and presence of an S3 heart sound. In patients where the diagnosis of MI is uncertain, radiation of pain
to the shoulder OR both arms, radiation to the
right arm, and vomiting had the best predictive values, while radiation to the left arm is relatively non-diagnostic.
Complications of MI
CRASH PAD
Cardiac Rupture
Arrhythmia
Shock
Hypertension/Heart failure Pericarditis/Pulmonary emboli Aneurysm
DVT
Resting LVEF is a useful prognostic factor
Enoxaparin vs. Unfractionated Heparin with Fibrinolysis for ST-elevation Myocardial Infarction
NEJM 2006;354:1477-1488
Study: Prospective multicentre RCT.
Patients: 20,479 patients (median age 60 yr, 77% male) with STEMI who were scheduled to undergo fibrinolysis.
Intervention: Patients were randomized to receive either enoxaparin or weight based unfractionated heparin in addition to thrombolysis and standard therapies.
Primary Outcome: Death or recurrent nonfatal MI 30 d post-event.
Results: The composite primary outcome occurred less often in the enoxaparin group compared with those who received unfractionated heparin (9.9% vs. 12.0%, p<0.001, NNT=47). Taken separately, there was a trend toward reduced mortality (6.9% vs. 7.5%, p=0.11) and a significant reduction in nonfatal reinfarction (3.0% vs. 4.5%, p<0.001) in the enoxaparin group. The risk of major bleeding was significantly increased in the enoxaparin group (2.1% vs. 1.4%, p<0.001, NNH=142). Conclusion: In patients with STEMI receiving thrombolysis, enoxaparin is superior to unfractionated heparin in preventing recurrent nonfatal MI and may lead to a small reduction in mortality.
High Risk (30-35%)
• Prior MI
• CHF
• Recurrent Ischemia • High-Risk Arrhythmia
Cardiac Catheterization *note: echo done routinely post-MI
Figure 37. Post-MI risk stratification
Prognosis following STEMI
• 5-15%ofhospitalizedpatientswilldie ■ risk factors
◆ infarct size/severity
◆ age
◆ comorbid conditions
◆ development of heart failure or hypotension
• post-dischargemortalityrates
■ 6-8% within first year, half of these within first 3 mo ■ 4% per year following first yr
■ risk factors
◆ LV dysfunction
◆ residual myocardial ischemia ◆ ventricular arrhythmias
◆ history of prior MI
Table 9. Complications of Myocardial Infarction
Intermediate/Low-Risk (65-70%)
Non-Invasive Stress Testing
Ischemia or Poor Functional Status
Normal Results
No further testing at this time
Complication
Arrhythmia
1. Tachycardia 2. Bradycardia
Myocardial Rupture
1. LV free wall
2. Papillary muscle (→ MR)
3. Ventricular septum (→ VSD)
Shock/CHF Post-Infarct Angina
Recurrent MI
Thromboembolism Pericarditis Dressler’s Syndrome
Etiology
Sinus, AFib, VT, VFib Sinus, AV block
Transmural infarction Inferior infarction
Septal infarction
Infarction or aneurysm Persistent coronary stenosis Multivessel disease Reocclusion
Mural/apical thrombus DVT Inflammatory
Autoimmune
Presentation
First 48 h First 48 h
1-7 d
1-7 d
1-7 d Within 48 h Anytime
Anytime
7-10 d, up to 6 mo 1-7 d
2-8 wk
Therapy
See Arrhythmias, C16
Surgery
Surgery
Surgery
Inotropes, intra-aortic balloon pump Aggressive medical therapy
PCI or CABG
Aggressive medical therapy PCI or CABG Anticoagulation
ASA