Page 99 - TNFlipTest
P. 99
Toronto Notes 2019 Ischemic Heart Disease Treatment Algorithm for Chest Pain
Cardiology and Cardiac Surgery C31
Intensive vs. Moderate Lipid Lowering with Statins after Acute Coronary Syndromes NEJM 2004;350:1495-1504
Study: Prospective, double blind, RCT; mean follow-up of 2 yr.
Population: 4,162 patients who had been hospitalized for an ACS within the preceding 10 d. Intervention: Patients were randomized to receiving pravastatin 40 mg or atorvastatin 80 mg daily. Primary Outcome: Composite of death from any cause, myocardial infarction, documented unstable angina requiring rehospitalization, revascularization (performed at least 30 d after randomization),
and stroke.
Results: High dose atorvastatin was associated with a 16% hazard ratio reduction (p=0.005; 95% CI 5-26%) in the primary outcome compared to standard dose pravastatin.
Conclusions: In patients who recently experienced an ACS, high dose statin therapy provides greater protection against death and major cardiovascular events than standard dose therapy.
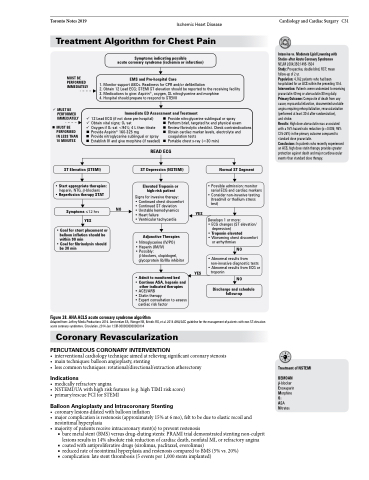
MUST BE PERFORMED IMMEDIATELY
Symptoms indicating possible
acute coronary syndrome (ischemia or infarction)
EMS and Pre-hospital Care
1. Monitor support ABCs. Readiness for CPR and/or defibrillation
2. Obtain 12 Lead ECG; STEMI ST elevation should be reported to the receiving facility 3. Medications to give: Aspirin®, oxygen, SL nitroglycerine and morphine
4. Hospital should prepare to respond to STEMI
Immediate ED Assessment and Treatment
MUST BE PERFORMED IMMEDIATELY
MUST BE PERFORMED IN LESS THAN 10 MINUTES
12 Lead ECG (if not done pre-hospital) Obtain vital signs; O2 sat
Oxygen if O2 sat <94%; 4 L then titrate Provide Aspirin® 160-325 mg
Provide nitroglycerine sublingual or spray Establish IV and give morphine (if needed)
Provide nitroglycerine sublingual or spray
Perform brief, targeted hx and physical exam
Review fibrinolytic checklist. Check contraindications Obtain cardiac marker levels, electrolyte and
ST Elevation (STEMI)
• Start appropriate therapies:
heparin, NTG, β-blockers
• Reperfusion therapy STAT
Symptoms ≤12 hrs YES
• Goal for stent placement or balloon inflation should be within 90 min
• Goal for fibrinolysis should be 30 min
READ ECG
ST Depression (NSTEMI)
Elevated Troponin or high-risk patient
Signs for invasive therapy:
• Continued chest discomfort • Continued ST deviation
• Unstable hemodynamics
• Heart failure
• Ventricular tachycardia
Adjunctive Therapies
• Nitroglycerine (IV/PO) • Heparin (IM/IV)
• Possibly:
β-blockers, clopidogrel, glycoprotein lib/IIIa inhibitor
YES
coagulation tests
Portable chest x-ray (<30 min)
NO
Normal ST Segment
• Possible admission: monitor serial ECG and cardiac markers
• Consider non-invasive testing (treadmill or thallium stress test)
YES
Develops 1 or more:
• ECG changes (ST elevation/
depression)
• Troponin elevated
• Worsening chest discomfort
or arrhythmias
NO
• Admit to monitored bed
• Continue ASA, heparin and
other indicated therapies
• ACEI/ARB
• Statin therapy
• Expert consultation to assess
cardiac risk factor
• Abnormal results from non-invasive diagnostic tests
• Abnormal results from ECG or troponin
NO
Figure 38. AHA ACLS acute coronary syndrome algorithm
Adapted from: Jeffery Media Productions 2016. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes. Circulation. 2014 Jan 1:CIR-0000000000000134
Coronary Revascularization
PERCUTANEOUS CORONARY INTERVENTION
• interventionalcardiologytechniqueaimedatrelievingsignificantcoronarystenosis • maintechniques:balloonangioplasty,stenting
• lesscommontechniques:rotational/directional/extractionatherectomy
Indications
• medicallyrefractoryangina
• NSTEMI/UAwithhighriskfeatures(e.g.highTIMIriskscore) • primary/rescuePCIforSTEMI
Balloon Angioplasty and Intracoronary Stenting
• coronarylesionsdilatedwithballooninflation
• majorcomplicationisrestenosis(approximately15%at6mo),felttobeduetoelasticrecoiland
neointimal hyperplasia
• majorityofpatientsreceiveintracoronarystent(s)topreventrestenosis
■ bare metal stent (BMS) versus drug-eluting stents: PRAMI trial demonstrated stenting non-culprit lesions results in 14% absolute risk reduction of cardiac death, nonfatal MI, or refractory angina
■ coated with antiproliferative drugs (sirolimus, paclitaxel, everolimus)
■ reduced rate of neointimal hyperplasia and restenosis compared to BMS (5% vs. 20%)
■ complication: late stent thrombosis (5 events per 1,000 stents implanted)
Treatment of NSTEMI
BEMOAN
β-blocker Enoxaparin Morphine O2
ASA Nitrates
Discharge and schedule follow-up